Environmental Psychopharmacology...
According to Golembiewski, the idea that the environment should make a difference in mental health has led to a possibly misguided trend to redecorate psychiatric facilities with the aim of making spaces more homely. However, as discussed earlier, this is at odds with the common thought that much if not most psychogenesis of mental illness occurs at home. However, what has been reinforced by recent studies is that psychiatric patients are much more reactive to the physical environment than healthy controls, which indicates that the environment is probably a good target for psychiatric interventions (Jan A Golembiewski.'A Review of Mental Health Facility Design: the Case for Person-Centred Care.' Australian & New Zealand Journal of Psychiatry (IN PRESS) 2014).
G proposes a prescription for 'psychopharmacology' in the form of patient centred spaces and 'designing the experience'.
Key points for designing the experience:
- psychiatric patients have amplified perceptions of their environment so the environment should be much better than merely domestic - it should exceed the expectations of the patient's experience by maximising (1) quality (2) choice of 'therapeutic' activities (3) aesthetic values (4) provisions for privacy, dignity and sanctuary, comprehensibility and meaningfulness.
- this will be a complex combination of things, not just (eg) colour or materials. Things that indicate a place is safe and nice (?) are: (1) open windows looking out over some natural landscape/water (2) comfortable furnishings (3) appropriately soft lighting (4) natural pleasant sounds and smells
- meaningful activities may include gardening, art, sports, music, kitchens they can use, computers with internet access
Layout of spaces: patient vs staff centred
Te tahuhu: Improving Mental Health 2005-2015: The Second New Zealand Mental Health and Addiction Plan (Ministry of Health, 2005) defines recovery in mental health in terms of a cultural change in services provided, plus an emphasis on the service being person-centred (rather than centred around the expertise of psychiatry).
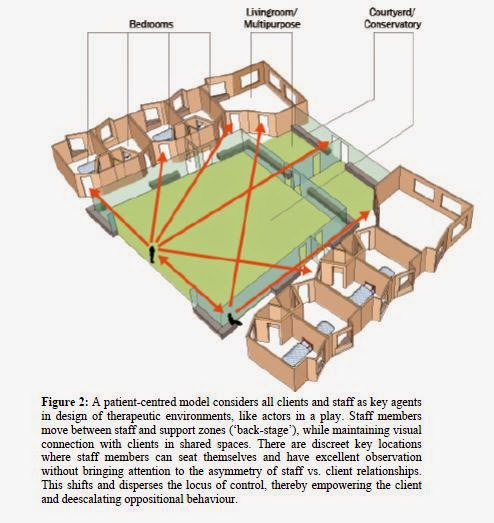
This is reflected in recent texts (including the one by Golembiewski) on how mental health units are generally still staff-centred with the nurses station being a central element in the design of these buildings. Golembiewksi proposes a more patient centred approach with patient spaces being privileged over staff spaces (Jan A Golembiewski.'A Review of Mental Health Facility Design: the Case for Person-Centred Care.' Australian & New Zealand Journal of Psychiatry (IN PRESS))

No comments:
Post a Comment